The field of regenerative medicine has witnessed a groundbreaking advancement with the development of cellular reprogramming therapies, particularly the conversion of skin cells into functional cardiomyocytes. This innovative approach holds immense potential for treating heart diseases, which remain a leading cause of mortality worldwide. By harnessing the plasticity of somatic cells, scientists are now able to bypass ethical concerns associated with embryonic stem cells while offering personalized therapeutic solutions.
The Science Behind Cellular Reprogramming
At the core of this revolutionary technique lies the process of direct lineage reprogramming, where adult skin fibroblasts are transformed into induced cardiomyocytes (iCMs) through the introduction of specific transcription factors. Pioneering work by researchers demonstrated that a combination of cardiac-specific genes—Gata4, Mef2c, and Tbx5—could effectively rewrite the cellular identity of fibroblasts. Unlike induced pluripotent stem cells (iPSCs), which require complete dedifferentiation, this method achieves transdifferentiation without reverting to a pluripotent state, significantly reducing tumorigenesis risks.
Recent refinements in the protocol have improved conversion efficiency from less than 1% to nearly 30% through optimized delivery systems and microenvironment conditioning. The advent of CRISPR-based gene editing has further enhanced precision, allowing scientists to activate endogenous cardiac programs while silencing fibroblast signatures. These technological leaps have transformed what was once considered science fiction into clinically viable procedures.
Overcoming Cardiac Regeneration Barriers
The human heart's limited regenerative capacity makes it particularly vulnerable to irreversible damage following myocardial infarction. Traditional treatments focus on managing symptoms rather than restoring lost tissue. Cellular reprogramming addresses this fundamental limitation by creating new functional heart muscle cells directly within the scar tissue. Animal studies have shown remarkable results—mice subjected to induced myocardial infarction exhibited improved ejection fraction and reduced fibrosis after receiving reprogrammed cardiomyocytes.
What makes this approach truly revolutionary is its potential for in situ reprogramming, where conversion occurs directly in the living heart without cell transplantation. Preliminary experiments demonstrate that viral vectors carrying reprogramming factors can transform cardiac fibroblasts into working cardiomyocytes when injected into damaged areas. This eliminates complex cell isolation and expansion procedures while minimizing immune rejection risks.
Clinical Translation Challenges
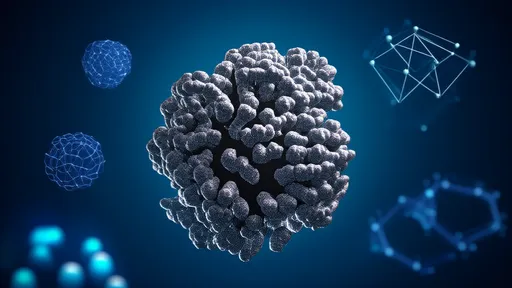
Despite promising preclinical results, several hurdles must be overcome before widespread clinical adoption. The incomplete maturation of reprogrammed cardiomyocytes remains a significant concern—while these cells exhibit electrical activity and contractility, they often resemble fetal rather than adult heart cells. Researchers are investigating various biochemical and biophysical cues to enhance maturation, including electrical stimulation and three-dimensional culture systems that better mimic native cardiac tissue.
Safety considerations also demand rigorous attention. Off-target effects of reprogramming factors could theoretically convert unintended cell types or create arrhythmogenic foci. Advanced delivery methods such as modified mRNA and nanoparticle systems are being developed to achieve transient, localized expression of reprogramming factors. Additionally, the field must establish standardized protocols for characterizing the electrophysiological properties and long-term behavior of converted cells.
The Future of Personalized Cardiac Medicine
Perhaps the most exciting prospect of skin-to-heart reprogramming lies in its potential for personalized therapies. A patient's own skin cells could serve as an abundant, immunocompatible source for generating cardiomyocytes tailored to their specific genetic makeup. This becomes particularly relevant for genetic cardiac conditions, where corrected patient-specific cells could theoretically replace diseased tissue without triggering immune responses.
Looking ahead, researchers envision combining cellular reprogramming with tissue engineering to create bioartificial heart patches or even whole-organ replacements. The convergence of gene editing, biomaterials science, and cellular reprogramming technologies may eventually enable complete cardiac regeneration. As clinical trials progress from small animal models to large mammals and eventually humans, the medical community watches with cautious optimism.
The ethical and regulatory landscape surrounding this technology continues to evolve alongside the science. While cellular reprogramming avoids the embryo destruction controversy of earlier stem cell therapies, it introduces new questions regarding genetic modification and long-term cellular behavior. Transparent dialogue between scientists, ethicists, and policymakers will be crucial as these treatments move toward clinical reality.
From bench to bedside, the journey of cellular reprogramming therapy exemplifies the transformative power of fundamental biological discovery. What began as basic research into developmental biology has blossomed into a potential paradigm shift for treating heart disease. While significant work remains, the prospect of regenerating damaged hearts through cellular alchemy represents one of the most promising frontiers in modern medicine.

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 10, 2025

By /Jul 10, 2025

By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 9, 2025